
Dan Carter, ND
Diabetes in America1
From 2001 to 2020, diabetes rates increased significantly among US adults older than 18.
- 37.3 million people have diabetes— 11.3% of the US population.
- 28.7 million people have been diagnosed with diabetes.
- 8.5 million people who have diabetes have not been diagnosed and do not know they have it.
- The rate of new cases of diabetes in the younger than 20-year age group increased in the United States between 2002 and 2015, with a 4.8% increase per year for type 2 diabetes and a 1.9% increase per year for type 1 diabetes.
Prediabetes
- Before developing type 2 diabetes, most people go through a prediabetic phase; their blood sugar is higher than normal but not high enough for a diabetes diagnosis. Prediabetes is common
- 96 million US adults have prediabetes.
- 26.4 million adults 65 or older have prediabetes.
Pathophysiology of Hyperglycemia
Hyperglycemia is blood glucose greater than 125 mg/dL fasting and greater than 180 mg/dL 2 hours postprandial. Impaired glucose tolerance, or pre-diabetes, is defined by a fasting plasma glucose of 100 mg/dL to 125 mg/dL. Untreated hyperglycemia leads to many serious life-threatening complications that include damage to the eye, kidneys, nerves, heart, and peripheral vascular system. It is vital to manage hyperglycemia effectively and quickly, to prevent complications of the disease and improve patient outcomes2.
Hyperglycemia in a patient with type 1 diabetes results from genetic, environmental, and immunologic causes. These lead to the destruction of pancreatic beta cells and insufficient insulin. In a patient with type 2 diabetes, insulin resistance and abnormal insulin secretion cause hyperglycemia.
Evolving data suggest a role for adipokine dysregulation, inflammation, and abnormalities in gut microbiota. Also, immune dysregulation, and inflammation have emerged as important pathophysiological factors.3
Hyperglycemia leads to extraordinary levels of oxidative stress! Oxidative stress, hyperglycemia, and pro-inflammatory processes feedback with each other and increase those conditions. These processes damage cellular structures, finally giving place to a progressively greater degree of oxidative stress with further hyperglycemia, metabolic alterations, and diabetes complications such as vascular damage.4
The high-calorie western diet contains large amounts of fats and carbohydrates that elevate blood glucose, very-low-density lipoproteins (VLDLs), chylomicrons (CMs) and chylomicron remnants (CMRs) that are rich in triglycerides (TG). This results in a spike of reactive oxygen species (ROS) concentrations, which in turn leads to an abnormal generation of inflammatory molecules.5 This diet, when consumed chronically, contributes to the high prevalence of metabolic syndrome (MetS) in the United States; NHANES data from 2011-2016 showed MetSprevalence was 19.5% among those aged 20 to 39 years, increasing to 48.6% among those aged 60 years.6 MetS includes central obesity, hypertension, insulin resistance and dyslipidemia. It is clearly associated with an increased risk of developing complications such as diabetes and atherosclerotic cardiovascular disease.7
Diagnosis of type 2 diabetes
If is recommended that one of the following plasmaglucose tests be performed in addition to hemoglobin A1c: Results are diagnostic for type 2 diabetes.
- Fasting plasma glucose:126 mg/dL or higher
- 2-hour plasma glucose level of 200 mg/dL or higher after a 75-g oral glucose challenge
- Random plasma glucose of 200 mg/dL or higher with symptoms of hyperglycemia
- Hemoglobin A1c level of 6.5% or higher
Lifestyle Management Overview
Patients with type 2 diabetes are faced with a life-long challenge to maintain normal blood sugars. They must be educated to make changes in their lifestyle that can significantly improve their prognosis.
Diet
Diet has more beneficial, or harmful, effects on type 2 diabetes than any other intervention.
What is a bad diet and why does it cause harm?
- Diets that lead to metabolic disease, including hyperglycemia/diabetes, are high in fat and carbohydrates, and may be low in protein. Many of the carbohydrates are simple sugars or highly processed carbohydrate-rich foods. High carbohydrate consumption requires high levels of insulin production in order to move the glucose from the blood into the cells, where it is converted to energy in the Krebs Cycle. In the case of the liver, excess glucose is metabolized to triglycerides, which are transported to liver cells, adipocytes, and muscle tissue, and stored.
- Fat stored in the liver results in non-alcoholic fatty liver disease (NAFLD), which is a leading cause of cirrhosis and hepatocellular carcinoma. NAFLD has a global prevalence of 25%.8
- Insulin resistance is primarily an acquired condition related to excess body fat; the primary drivers of insulin resistance are the liver, skeletal muscle, and adipose tissue. Hyperinsulinemia leads the body into a storage mileiu, where fat is preferentially stored and glucose is the primary fuel for energy. Fat will not be mobilized from adipose tissue as long as insulin is high.9
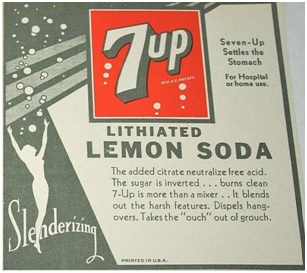
7up Logo from 1929
What is an effective diet for regaining metabolic health?
- Nutritional intervention involving calorie reduction and avoidance of carbohydrates that stimulate excessive insulin demand is a cornerstone of treatment.
- Metabolic health is adversely affected by NAFLD. A very low calorie ketogenic diet is effective in reducing visceral and liver fat accumulation.10
- Well-formulated Ketogenic diets are effective for glucose control, decreasing insulin resistance, and weight loss that improves body composition, e.g. retaining muscle mass while loosing body fat. Eric Westman, MD, is a good resource for learning about Ketogenic Diets. He is a researcher and co-author of studies regarding the diet in peer-reviewed literature.111213 https://adaptyourlifeacademy.com/
Physical activity
- Physical activity increases energy expenditure and improves skeletal muscle insulin sensitivity.
- Sport and exercise trigger adaptation and repair mechanisms in organ systems and cells, including muscles, nerves, blood vessels, immune system and brain.
- Diabetic adults should exercise for 150 minutes/week or more at moderate intensity. A recent study showed that 7000-9000 steps daily, at moderate to high cadence, helped decrease all cause mortality and cardiovascular events.14
- Strength training 2–3 times a week is also essential, but not on consecutive days. Interrupt periods of sitting every 30 minutes.
- More than 2 consecutive days of inactivity can initiate a trend that leads to loss of previous exercise benefit.15
At IV Nutritional Therapy, our mission is to teach safe and effective ways to administer intravenous micro-nutrients and pharmaceuticals. We provide education seminars across the globe for medical professionals.
If you want to learn more about our upcoming seminars and educational materials, visit www.IVNutritionalTherapy.com or contact us here.
1From the website: https://www.innerbody.com/diabetes-statistics-in-the-united-stateshttps://www.cdc.gov/diabetes/health-equity/diabetes-by-the-numbers.html. Accessed 12 November 2024.
2Mouri MI, Badireddy M. Hyperglycemia. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430900/
3Schwartz S.S., Epstein S., Corkey B.E., et al. The Time Is Right for a New Classification System for Diabetes: Rationale and Implications of the beta-Cell-Centric Classification Schema. Diabetes Care. 2016;39:179–186. doi: 10.2337/dc15-1585.
4González P, Lozano P, Ros G, Solano F. Hyperglycemia and Oxidative Stress: An Integral, Updated and Critical Overview of Their Metabolic Interconnections. Int J Mol Sci. 2023 May 27;24(11):9352. doi: 10.3390/ijms24119352. PMID: 37298303; PMCID: PMC10253853.
5Galicia-Garcia U, Benito-Vicente A, Jebari S, et al. Pathophysiology of Type 2 Diabetes Mellitus. Int J Mol Sci. 2020 Aug 30;21(17):6275. doi: 10.3390/ijms21176275. PMID: 32872570; PMCID: PMC7503727.
6Hirode G, Wong RJ. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011-2016. JAMA. 2020;323(24):2526–2528. doi:10.1001/jama.2020.4501
7Rochlani Y., Pothineni N.V., Kovelamudi S., Mehta J.L. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 2017;11:215–225. doi: 10.1177/1753944717711379.
8Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease. Lancet. 2021 Jun 5;397(10290):2212-2224. doi: 10.1016/S0140-6736(20)32511-3. Epub 2021 Apr 21. PMID: 33894145.
9Freeman AM, Acevedo LA, Pennings N. Insulin Resistance. [Updated 2023 Aug 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507839/
10Cunha GM, Guzman G, Correa De Mello LL, et al. Efficacy of a 2-Month Very Low-Calorie Ketogenic Diet (VLCKD) Compared to a Standard Low-Calorie Diet in Reducing Visceral and Liver Fat Accumulation in Patients With Obesity. Front Endocrinol (Lausanne). 2020 Sep 14;11:607. doi: 10.3389/fendo.2020.00607. PMID: 33042004; PMCID: PMC7521128.
11Yancy WS Jr, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med. 2004 May 18;140(10):769-77. doi: 10.7326/0003-4819-140-10-200405180-00006. PMID: 15148063.
12Feinman RD, Pogozelski WK, Astrup A, Bernstein RK, Fine EJ, Westman EC, Accurso A, Frassetto L, Gower BA, McFarlane SI, Nielsen JV, Krarup T, Saslow L, Roth KS, Vernon MC, Volek JS, Wilshire GB, Dahlqvist A, Sundberg R, Childers A, Morrison K, Manninen AH, Dashti HM, Wood RJ, Wortman J, Worm N. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015 Jan;31(1):1-13. doi: 10.1016/j.nut.2014.06.011. Epub 2014 Jul 16. Erratum in: Nutrition. 2019 Jun;62:213. PMID: 25287761.
13Westman EC, Tondt J, Maguire E, Yancy WS Jr. Implementing a low-carbohydrate, ketogenic diet to manage type 2 diabetes mellitus. Expert Rev Endocrinol Metab. 2018 Sep;13(5):263-272. doi: 10.1080/17446651.2018.1523713. PMID: 30289048.
14Stens NA, Bakker EA, Mañas A, et al. Relationship of Daily Step Counts to All-Cause Mortality and Cardiovascular Events. J Am Coll Cardiol. 2023 Oct 10;82(15):1483-1494. doi: 10.1016/j.jacc.2023.07.029. Epub 2023 Sep 6. PMID: 37676198.
15Esefeld K, Kress S, Behrens M, Zimmer P, Stumvoll M, Thurm U, Gehr B, Brinkmann C, Halle M. Diabetes, Sports and Exercise. Exp Clin Endocrinol Diabetes. 2021 Aug;129(S 01):S52-S59. doi: 10.1055/a-1284-6097. Epub 2020 Dec 21. PMID: 33348380.


Hi, I’m Jack. Your website has become my go-to destination for expert advice and knowledge. Keep up the fantastic work!
Thanks I have recently been looking for info about this subject for a while and yours is the greatest I have discovered so far However what in regards to the bottom line Are you certain in regards to the supply